A study of over 41,000 patients showed inpatient mortality almost doubles when emergency department (ED) throughput stretches from 2 hours to more than 12 hours. Meanwhile, excess inventory and poor purchasing decisions inflate non-labor expenses by an estimated $200 billion per year—enough to fund 2,000 community hospitals.
Hospitals aren't stuck from a lack of innovation—they’re stuck because yesterday’s strengths became today’s constraints.
Legacy org charts, misaligned incentives, and slow-motion governance let queues, waste, and burnout expand until they threaten an entire system’s viability.
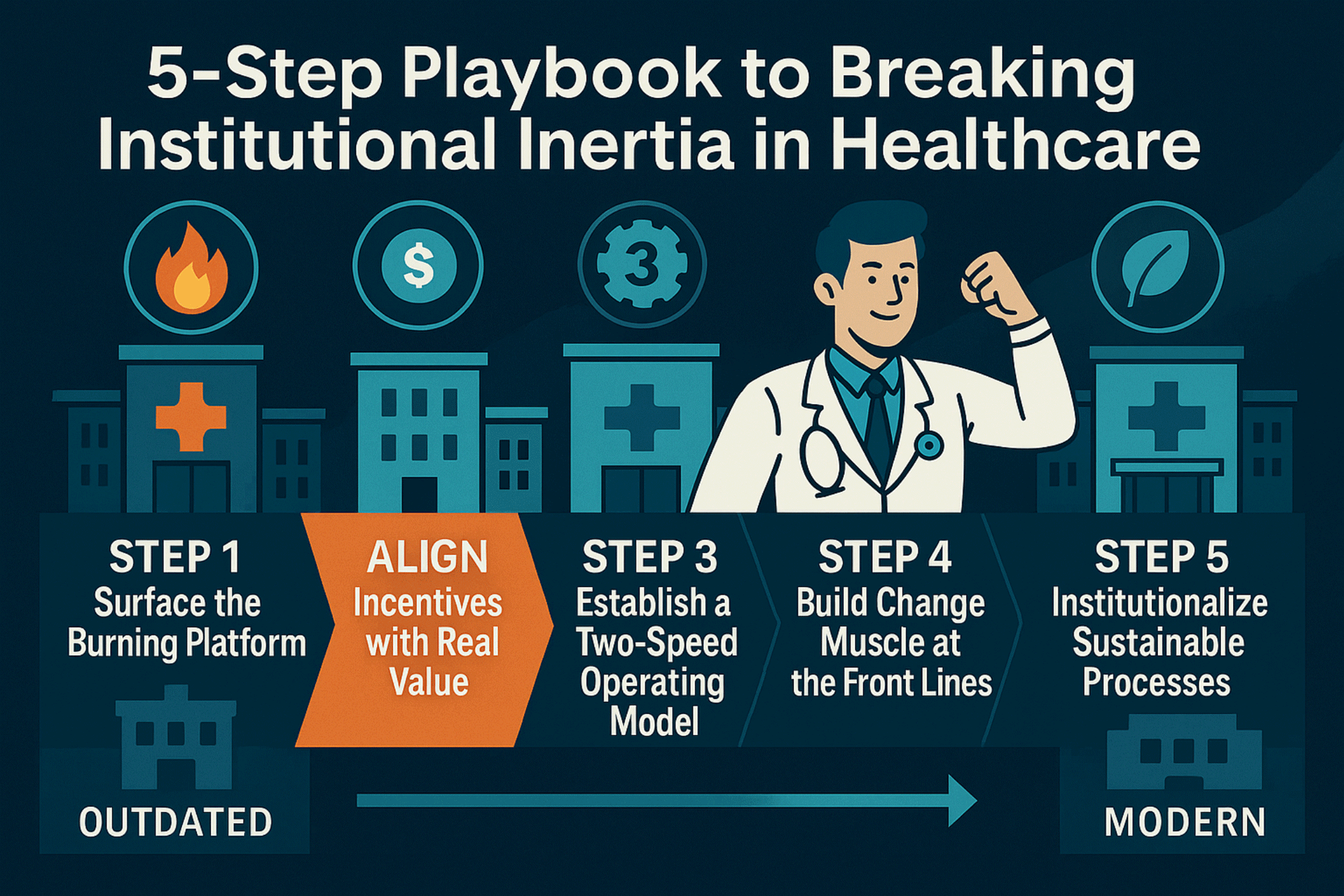
This five-step playbook equips C-suite leaders, including Chief Supply Chain Officers (CSCOs), to identify and dismantle bottlenecks, sharpen the right metrics, and hardwire a culture that keeps getting faster, safer, and more cost-effective.
5-Step Roadmap to Break Institutional Inertia in Healthcare
1. Expose the Burning Platform with the Right Measures
- Replace vanity metrics with impact metrics. Most hospitals track outputs (beds filled) instead of flow signals (boarding minutes), so blind spots multiply until they hurt patients. Swap “beds filled” and “OR minutes booked” for average LOS, ED boarding time, readmissions, patient-reported satisfaction, nursing overtime, and inventory turns.
- Quantify the price tag of constraints. Show how a one-hour reduction in average ED boarding can free 20+ staffed beds, slash overtime, and avert avoidable deaths.
- Tie dollars to lives. Link every day of excess length-of-stay (LOS) to net margin erosion and patient harm risk. Data plus human stories cut through inertia far faster than spreadsheets alone.
2. Realign Metrics, Incentives & Budgets Around True Value
- Flow-first scorecards. Give each service line a “Flow Index” (LOS, boarding hours, on-time starts, satisfaction) and weight it higher than sheer volume.
- Shared savings that matter. Tie leadership bonuses and physician comp to margin per encounter, supply cost per case, and patient experience scores— not Relative Value Units (RVUs) in isolation.
- Supply chain KPIs on every dashboard. Track SKU reduction, contract compliance rate, and purchase-price variance next to clinical quality. Visibility converts skeptics quickly.
3. Run a Two-Speed Operating Model That Targets the Bottleneck
- Core operations stay steady; a “Flow Lab” iterates in parallel. The Flow Lab uses predictive analytics, constraint mapping, and rapid cycle PDSA tests to attack whichever node is capping throughput (e.g., imaging turnaround, bed assignment, discharge approvals).
- Tip: Think of the concept of a Flow Lab like a permanent Kaizen blitz: each morning a cross-functional huddle selects the day’s top constraint, launches a 24- to 72-hour experiment in a sandbox, then locks in the win or pivots—compounding gains without disrupting care.
- Shield pilots from red tape. Grant same-day approvals, microbudgets, and direct C-suite access so frontline teams can elevate a stuck decision within 60 minutes.
- Exploit, synchronize, and expand.
- Exploit – Squeeze every ounce of output from the current choke point by streamlining tasks and eliminating idle minutes.
- Synchronize – Align every upstream and downstream schedule, staffing plan, and supply drop to keep that step fed and flowing—no starved time, no pileups.
- Expand – If it’s still the system’s slowest link, add capacity, redesign the workflow, or outsource pieces until it’s no longer the bottleneck.
- Cincinnati Children’s avoided building a $100M tower by leveling elective demand, freeing 100 beds, and adding $137M in annual revenue.
- Leading systems like Mayo and the Cleveland Clinic have explored dual-track innovation models to balance stability and rapid cycle improvement, particularly in OR throughput and AI-enabled forecasting areas.

4. Build Front Line Constraint Busting Muscle
- Equip charge nurses, unit clerks, periop leads, and supply coordinators with simple daily tools. Real-time constraint boards, 15-minute huddles, and an escalation tree that auto-pages the next level when boarding time > 90 minutes or PAR cart fill errors > 2%.
- Use near-real-time dashboards. If a bottleneck reappears, staff see it within hours, not quarters, enabling same-shift fixes.
- Reward action. Celebrate the team that shaved two hours off discharge paperwork or cut supply waste by 12%; tell their story in every town hall or system-wide educational event.
5. Hardwire & Monitor the Gains
- Embed rules in the EHR, ERP, and contracts. Examples include auto-cancelling unneeded and/or recurring labs; requiring an item master crosswalk before a new SKU can be ordered; locking discharge rounds by or before 9:00 am daily, for example.
- Governance with teeth. A monthly Flow Council reviews constraint metrics, assigns owners, and can reallocate capital within one meeting.
- Continuous improvement loop. When today’s constraint moves, the system instantly spots—and attacks—the next one.
Quick Wins to Prove the Concept in 90 Days
Days 1–30
✓ Clean the item De-duplicate SKUs, attach contract price, and flag critical items.
✓ Baseline LOS & boarding. Six weeks of historical data is enough.
Days 31–60
✓ Create an ED-to-Bed escalation tree. Example: >90 min: charge nurse escalates to bed management. >120 min: duty administrator auto-alert. >180 min: C-suite text + Flow Lab stand-up.
✓ Run a demand-leveling pilot in one service line (e.g., diagnostics) and measure the effect on nursing overtime and patient delays.
Days 61–90
✓ Publish a Flow Scoreboard in every break room: LOS, boarding hours, supply cost per discharge, patient satisfaction trend.
✓ Declare sunset dates for obsolete procedures (paper order sets, duplicate cart locations) and stick to them.

From Insight to Action
Institutional inertia isn’t a system glitch—it’s a leadership choice. The physics of queuing are clear, the financial upside is measurable, and competitors are already moving .
Three steps to move from inertia to impact this quarter:
- Measure what you control. LOS drivers, boarding triggers, supply spend, and revenue leakage.
- Bake flow and cost KPIs into next year’s budget. Not just volumes—balance, consistency, and satisfaction.
- Stand up a Flow Lab with real authority. Give it air cover, same day decision rights, and a direct line to the C-suite.
Call to Action: Break the Cycle. Lead the Shift. Start Transforming Today.
Input your email into the form below to request the following at no cost to your organization:
✓ Inventory data assessment
✓ Supply chain item master data assessment
✓ Leading practice supply chain resilience assessment
✓ Comprehensive healthcare performance improvement “control tower” KPIs
✓ Supplier Relationship Management (SRM) KPIs
Let BlueBin help you level your flow, free your people, and fund your future. Our transformation programs accelerate outcomes in 7–15 months, not the 3–5 YEARS most providers face when attempting to transform alone. And with a typical ROI in just 6–12 months, BlueBin's payoff is fast, measurable, and lasting.
