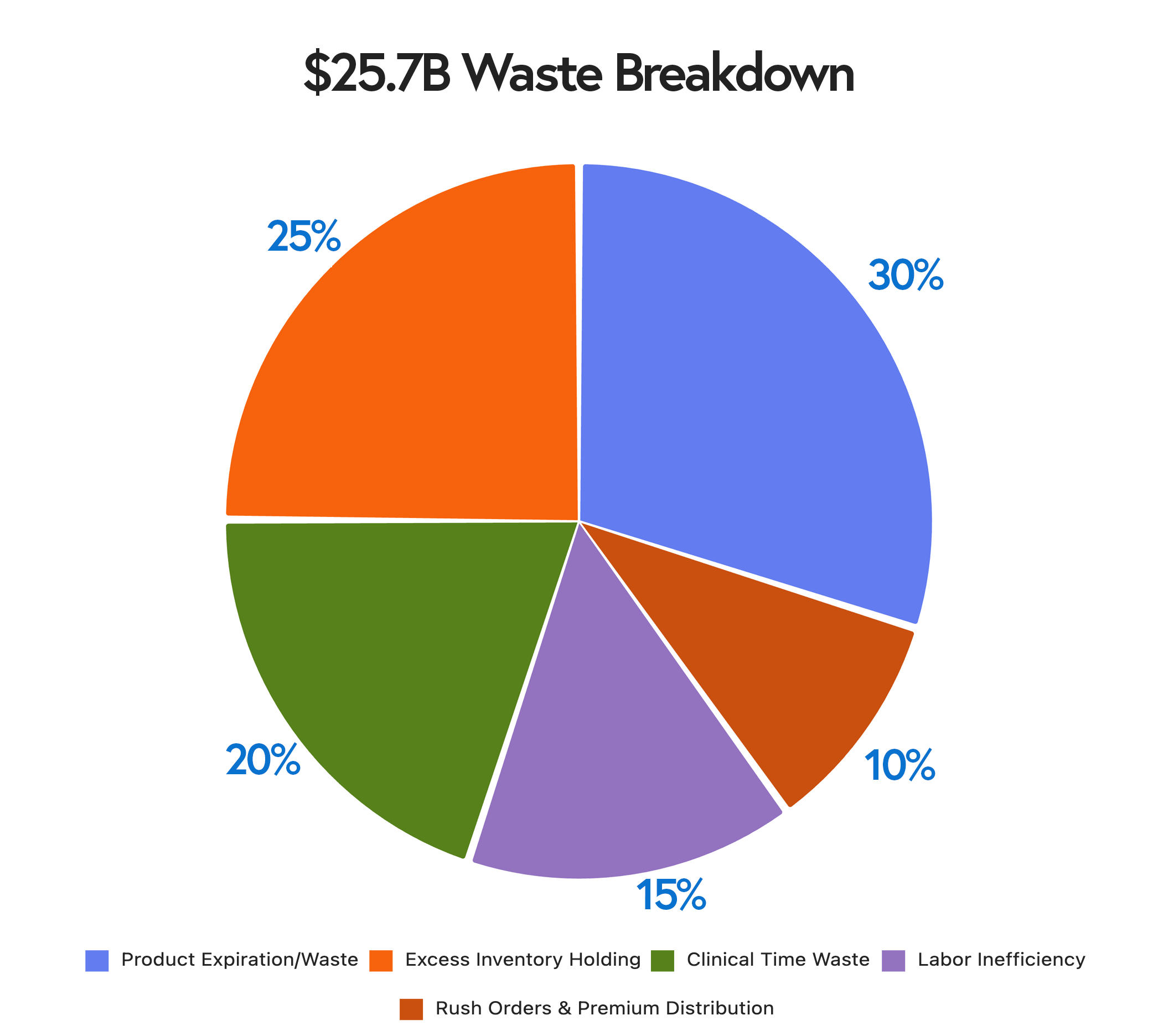
Purchase price is only the tip of the iceberg. Discover the hidden costs of healthcare supply chain inefficiency—inventory holding, clinical time waste, and more—totaling $25.7B annually.
When healthcare CFOs review supply chain performance, they typically focus on purchase price variance, contract compliance, and rebates from group purchasing organizations. These visible costs dominate budget discussions and performance scorecards. But like an iceberg, the purchase price floating visibly above the waterline represents only a fraction of the total cost.
Below the surface lurks a massive hidden expense structure that most healthcare organizations fail to measure, let alone manage. The industry wastes an estimated $25.7 billion annually on supply chain inefficiencies that are not reflected as line items in purchasing reports.
Understanding and addressing these hidden costs is the difference between managing supplies and transforming supply chain economics.
The Visible Costs: What Everyone Measures
Let's start with what's visible and what nearly every healthcare supply chain organization already tracks religiously:
Purchase Price: The actual price paid for medical supplies, pharmaceuticals, and equipment. This is the number that appears on invoices and purchase orders.
Contract Compliance: Whether the organization is purchasing at negotiated contract rates rather than paying premium prices for off-contract purchases.
Group Purchasing Organization (GPO) Performance: Rebates and administrative fees associated with GPO relationships.
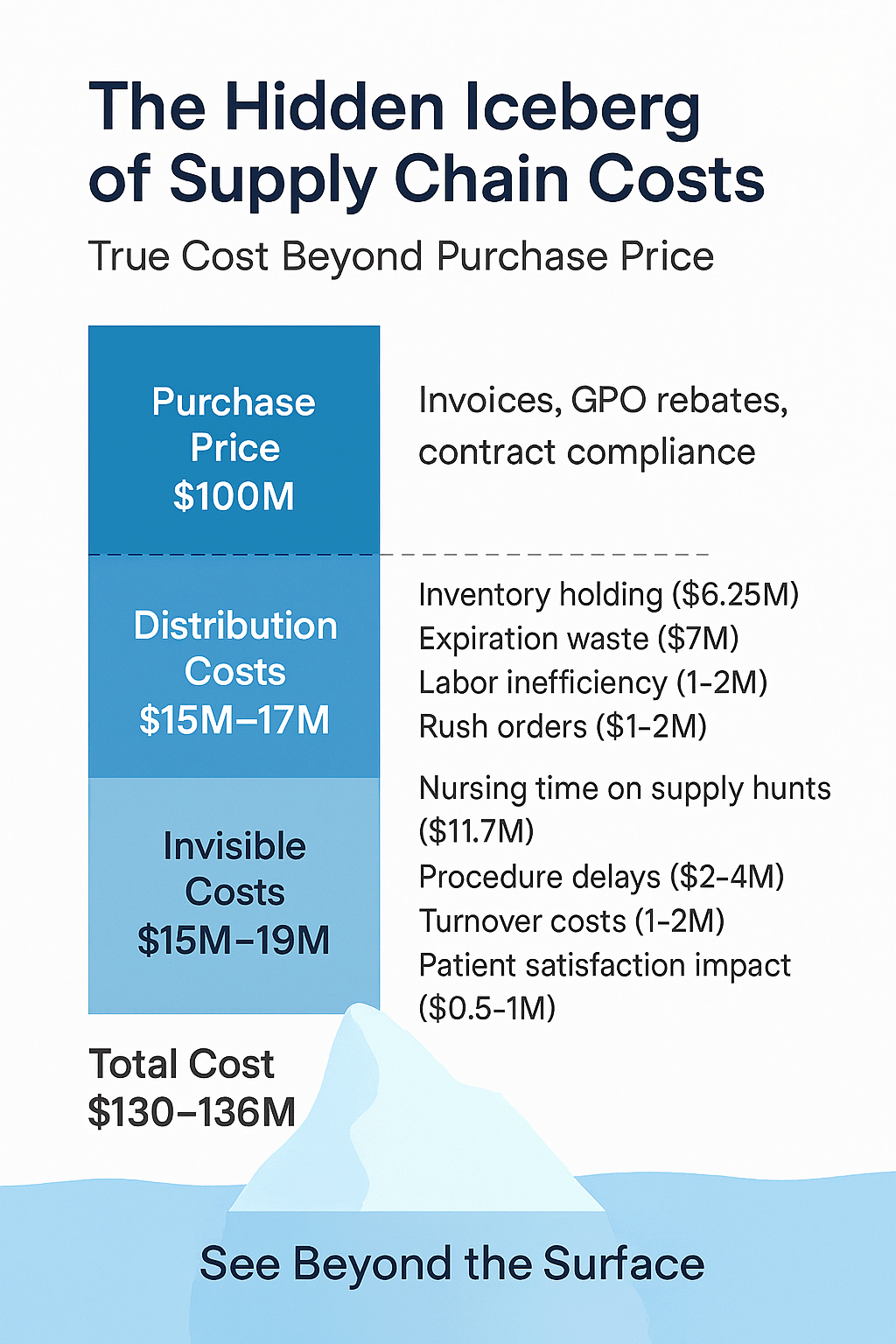
These costs matter immensely. A 2-3% improvement in purchase price for a hospital spending $100 million annually on supplies represents $2-3 million in savings. Supply chain teams rightly focus significant effort on negotiating better contracts, ensuring compliance, and optimizing GPO relationships.
However, here's the problem: these visible costs typically account for only 30-40% of the total cost of healthcare supply chain operations. The remaining 60-70%, distribution costs and invisible costs, often receive little attention because they're harder to quantify and don't appear as obvious line items in financial reports.
The Hidden Costs: Distribution and Management
Just below the waterline of purchase price lies the next layer of cost: the expenses associated with how supplies are distributed, managed, and stored within your organization.
Inventory Holding Costs
Healthcare organizations typically carry 20-30% of annual supply spend in inventory at any given time. A hospital spending $100 million on supplies annually may have $20-30 million worth of supplies sitting on shelves.
The carrying cost of that inventory, the actual expense of maintaining it, runs between 20% and 30% annually. This includes:
- Physical space costs (storage areas that could be used for revenue-generating purposes)
- Insurance
- Obsolescence and expiration (8-10% industry norm, reduced to <1% with proper management)
- Capital cost (the opportunity cost of money tied up in inventory rather than invested elsewhere)
- Management and handling
For our example hospital: $25M inventory × 25% carrying cost = $6.25 million annually to hold supplies on the shelf.
Most healthcare finance teams don't calculate or track this number explicitly. It's distributed across multiple budget lines (facilities costs, labor costs, write-offs) making it invisible in aggregate despite being larger than many obvious cost categories.
Distribution Labor Costs
Moving supplies from receiving to storage to point-of-use locations requires significant labor. Supply chain coordinators, materials management staff, and department-based employees all spend time on supply distribution activities.
Organizations using manual par cart systems or ad-hoc replenishment typically deploy 30-50% more labor than necessary. The waste comes from:
- Guessing at par levels rather than using data-driven optimization
- Multiple trips to the exact location due to stock-outs
- Emergency deliveries that interrupt planned routes
- Manual counting and documentation (83% of clinicians still count manually)
- Redundant handling and double-checking
For our example hospital, eliminating just 30% of wasted distribution labor could save $1-2 million annually in direct labor costs, as well as significant indirect costs resulting from better resource allocation.
Product Expiration and Waste
The average product expiration rate in the healthcare industry is 8-10%. For organizations with poor visibility and manual processes, it can be significantly higher. Organizations with excellent supply chain management reduce expirations to less than 1%.
For our example hospital: Reducing expirations from 8% to <1% saves approximately $7 million annually (7% of $100 million spent) in direct product waste, plus the labor cost of managing expired products and the patient safety risk of using near-expired supplies.
Rush Orders and Premium Distribution
When supplies aren't available when needed, organizations pay premiums for expedited delivery. Same-day vendor deliveries, courier services, and emergency purchases from local sources all carry significant premiums over routine distribution.
Research shows that 69% of perioperative staff have had to delay a case due to tracking down missing supplies. Each of these incidents generates rush order costs, procedure delays, and operational disruption.
Space Utilization
Hospital space commands premium pricing, often $400-$600 per square foot to build and $50-$100 per square foot annually to operate. Excess inventory occupies space that could be utilized to generate revenue through patient care areas, procedure rooms, or clinics.
Organizations that reduce inventory by 20-30% through better management often reclaim 1,000-3,000 square feet of storage space per facility. Converted to revenue-generating space, this can represent significant value.
The Invisible Costs: Clinical Time and Operational Disruption
Below the waterline of distribution costs lies the deepest and most expensive layer: the invisible costs of clinical time spent on supply management rather than patient care.
Supply Hunting by Clinicians
Perhaps the most shocking statistic in the healthcare supply chain: nurses waste up to 60 minutes per shift hunting for supplies. In a 12-hour shift, one hour is lost to supply searches rather than patient care.
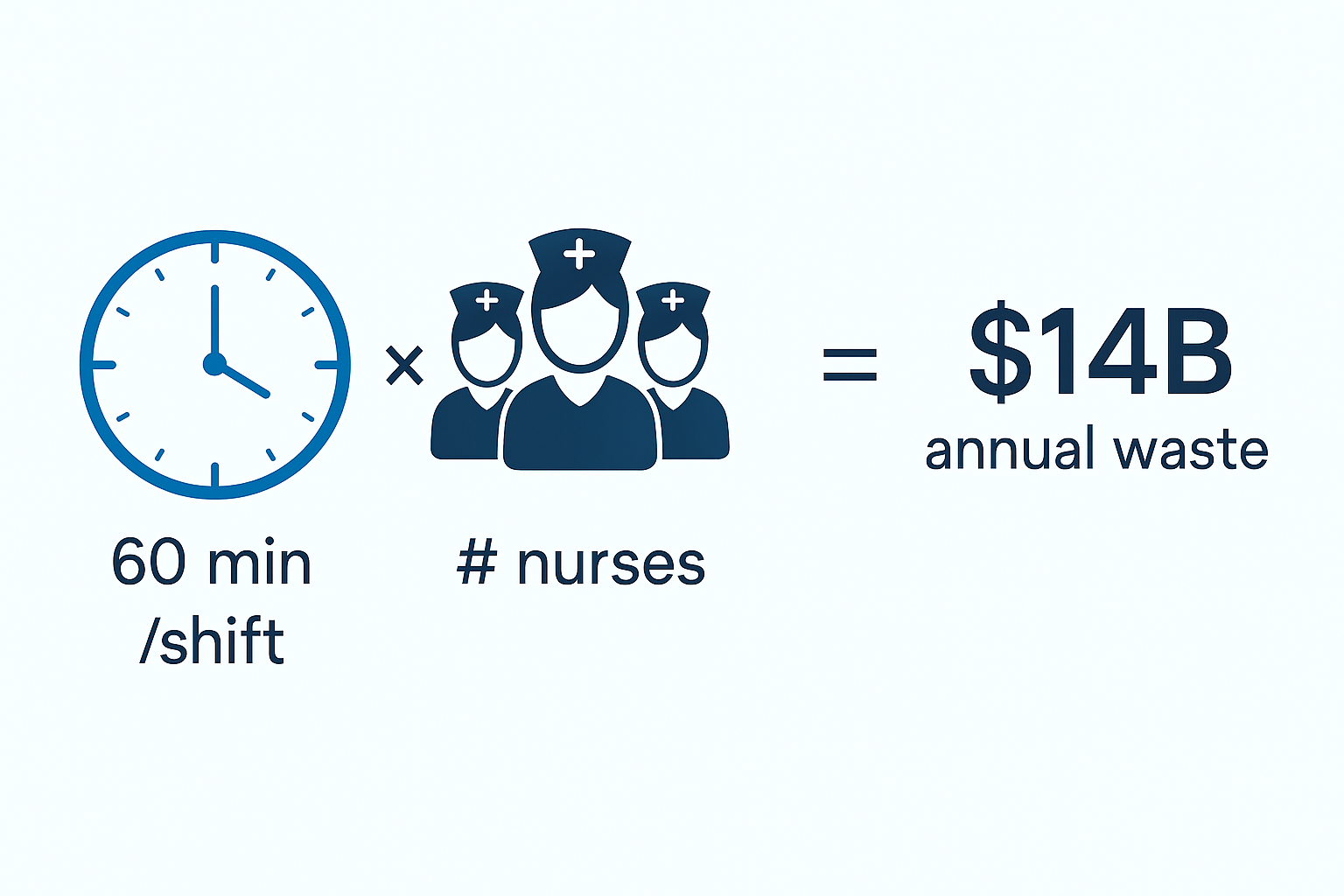
The cost is staggering. With approximately 3 million nurses in the United States earning an average of $35-45 per hour, the aggregate cost of supply hunting reaches $14 billion annually across the industry.
For a typical 300-bed hospital with 800 nursing FTEs:
- 800 nurses × 0.5 hours per shift × 365 days × 2 shifts/day = 292,000 hours annually
- 292,000 hours × $40/hour = $11.7 million in nursing time wasted on supply hunts
This cost dwarfs the purchase price savings that supply chain teams typically pursue. Yet because it doesn't appear as a supply chain line item (it's buried in nursing labor costs) it rarely factors into supply chain investment decisions.
Procedure Delays and Cancellations
Stock-outs don't just inconvenience clinicians, they delay and sometimes cancel procedures. Research indicates that 40% of healthcare staff have cancelled a case due to a lack of supplies.
Each cancelled or delayed procedure represents:
- Lost revenue from the procedure itself
- OR time that can't be recovered
- Patient dissatisfaction and potential safety issues
- Staff frustration and inefficiency
The financial impact is difficult to quantify precisely because hospitals don't typically track procedure delays specifically attributable to supply issues. However, conservative estimates suggest that millions of dollars in lost revenue are incurred annually by mid-sized hospitals.
Staff Satisfaction and Retention
Supply chain problems directly impact nurse satisfaction. When Press Ganey surveys at Ohio State University-Wexner Medical Center asked nurses about dissatisfaction factors, "I have the supplies I need to do my job" ranked in the top 10 concerns.
In an industry facing severe nursing shortages, anything that impacts nurse satisfaction has profound financial implications. The cost to replace a single nurse ranges from $40,000-$60,000. If poor supply availability contributes to even a 2-3% increase in nurse turnover, the financial impact for a 300-bed hospital could exceed $1 million to $2 million annually.
Organizations that achieve Magnet status, which requires demonstrating nurse satisfaction and excellent clinical outcomes, consistently cite supply chain excellence as a contributing factor. Einstein Medical Center specifically identified supply chain transformation as the "#1 contributing factor to achieving Magnet status."
Patient Satisfaction and Clinical Outcomes
When nurses spend time hunting for supplies instead of caring for patients, both patient satisfaction and clinical outcomes suffer. Press Ganey data shows that nurse responsiveness, their ability to be present and attentive to patient needs, is among the strongest predictors of overall patient satisfaction.
Patient satisfaction scores directly impact hospital reimbursement through value-based purchasing programs. A 5-point improvement in HCAHPS scores can be worth hundreds of thousands of dollars annually in additional Medicare payments for a mid-sized hospital.
The connection between supply chain performance and patient satisfaction is indirect but real: nurses who spend 50% less time hunting for supplies have more time for patient interaction, leading to better satisfaction scores and higher reimbursement.
The Total Cost: Adding It All Together
For our example hospital spending $100 million annually on medical supplies, the total cost structure looks like this:
Visible Costs (Above the Waterline):
- Purchase Price: $100 million
Distribution Costs (Just Below the Surface):
- Inventory Holding Costs: $6.25 million
- Excess Distribution Labor: $1-2 million
- Product Expiration: $7 million
- Rush Orders & Premium Distribution: $1-2 million
- Subtotal Distribution Costs: ~$15-17 million
Invisible Costs (Deep Below the Surface):
- Nursing Time on Supply Hunts: $11.7 million
- Procedure Delays/Cancellations: $2-4 million
- Incremental Turnover Costs: $1-2 million
- Patient Satisfaction Impact: $0.5-1 million
- Subtotal Invisible Costs: ~$15-19 million
Total Supply Chain Cost: $130-136 million
The purchase price of $100 million represents only 74-77% of the total economic cost of supply chain operations. The remaining $30-36 million in hidden costs, 30-36% of total cost, typically receives minimal attention because it's not tracked as "supply chain expense."
Why Organizations Fail to Address Hidden Costs
If hidden costs represent 30-36% of total supply chain economics, why don't more organizations focus on them?
Measurement Challenges
Hidden costs are genuinely difficult to measure. Nursing time on supply hunts doesn't appear as a line item. The cost of space occupied by excess inventory isn't calculated. Procedure delays attributed to supply issues aren't systematically tracked.
Without measurement, issues remain invisible. Without visibility, they don't get managed.
Organizational Silos
The supply chain owns the visible costs (purchase price). But the hidden costs are distributed across multiple departments:
- Nursing labor reports to CNO
- Facilities costs report to operations
- Patient experience teams own patient satisfaction
- Clinical outcomes fall under quality and safety
No single executive owns the total economic cost, so optimization of the complete picture rarely occurs.
Short-Term Thinking
Reducing the purchase price by 2-3% through aggressive negotiation can be achieved within a budget cycle. Addressing hidden costs through systematic transformation requires longer commitment and cross-functional collaboration.
Organizations default to what's measurable, achievable quickly, and within a single department's control, even when the bigger opportunity lies elsewhere.
The Transformation Opportunity
Healthcare organizations that systematically address hidden costs achieve extraordinary results. BJC HealthCare's transformation illustrates the magnitude:
Investment: $6.70 million over 36 months
Returns:
- $12.8 million annually in visible supply expense reduction (purchase price optimization)
- $5.8 million one-time inventory working capital release (inventory holding cost reduction)
- $1.9 million annually in resource redeployment (distribution labor optimization)
- Additional clinical time savings through a 50% reduction in supply hunts
Total ROI: 7.9x
The returns came from addressing the entire iceberg (visible costs, distribution costs, and invisible costs) not just negotiating better purchase prices.
What Supply Chain Leaders Should Do Differently
To capture the full value of supply chain optimization, leaders must:
Expand the Cost Model
Stop measuring supply chain performance solely by purchase price variance. Build comprehensive cost models that include:
- Inventory carrying costs
- Distribution labor efficiency
- Clinical time spent on supply management
- Space utilization
- Product waste
- Procedure disruption
This requires collaboration with finance, operations, and clinical leadership. The CFO needs to see the complete picture to make informed investment decisions.
Create Cross-Functional Accountability
Appoint someone, ideally at the C-suite level, to own total supply chain economics, not just purchasing. This role must have authority across silos to optimize the complete system, not just individual components.
Invest in Visibility
You can't manage what you can't measure. BlueQ Analytics and similar systems make hidden costs visible through:
- Real-time tracking of supply availability (revealing true cost of stock-outs)
- Heat maps showing problem areas (enabling targeted intervention)
- Labor time tracking (quantifying distribution efficiency)
- Expiration tracking (measuring waste)
- Daily huddle boards (creating accountability for total performance)
Make the Business Case for Comprehensive Transformation
When supply chain leaders ask for a budget to address only visible costs, they're competing for limited dollars. When they demonstrate that addressing hidden costs delivers 5-7x greater returns, the business case becomes compelling.
BJC HealthCare didn't invest $6.70 million to save 2-3% on purchase price. They invested to capture the entire opportunity, and achieved 7.9x ROI.
The Path Forward
The healthcare industry's $25.7 billion annual waste in supply chain operations isn't a mystery. It's hidden in plain sight, just below the waterline where most organizations don't look.
Supply chain leaders who illuminate these hidden costs and build the business case for comprehensive transformation create extraordinary value for their organizations. The returns come not from harder negotiating with vendors, but from fundamentally better systems that eliminate waste throughout the entire supply chain ecosystem.
The visible costs above the waterline matter. But the transformation opportunity lies below.
Ready to reveal your hidden supply chain costs? Request a comprehensive supply chain assessment to quantify your complete cost structure and identify transformation opportunities.
Related Resources:
- Total Cost of Supply Chain Calculator - Estimate Your Hidden Costs
- Case Study: BJC HealthCare's 7.9x ROI Transformation
FAQs
How can we calculate our specific hidden costs?
Start with these estimates and refine with your actual data:
- Inventory carrying cost: 20-30% of average inventory value
- Nursing time on supply hunts: 0.5 hours per nurse per shift × hourly rate × number of nurses × 730 shifts/year
- Expiration waste: Calculate write-offs as % of total supply spend
- Distribution labor excess: Estimate 20-40% waste in current labor deployment
Collaborate with finance and operations to develop your comprehensive model.
Which hidden costs should we address first?
Start with clinical time waste (supply hunts), as this typically delivers the most significant dollar impact and improves nurse satisfaction—a strategic priority for most organizations. Then address expiration waste and inventory holding costs. Distribution labor efficiency often comes last but still delivers significant value.
How do we get buy-in from nursing to address supply issues?
Frame it as giving nurses their time back for patient care. Nurses universally want to spend less time hunting for supplies and more time with patients. Supply chain transformation that delivers 30-50% fewer supply hunts is a nursing satisfaction initiative, not just a cost reduction program.
What's a reasonable timeline to address these hidden costs?
Comprehensive transformation that addresses visible costs, distribution costs, and invisible costs can be achieved in 9-15 months with a turnkey approach. Traditional internal programs typically take 3-5 years and often fail to address invisible costs.
How do we measure success if these costs are currently invisible?
Establish baselines before transformation:
- Survey nurses about the time spent on supply hunts
- Calculate current expiration rate
- Measure average inventory levels
- Document procedure delays attributed to supply issues
Then track these metrics monthly to demonstrate improvement. BlueQ Analytics automates much of this measurement.