Healthcare executives facing mounting cost pressures can't afford to wait 3 to 5 years for supply chain transformation results. Yet research from the Agency for Healthcare Research and Quality reveals that traditional lean programs consistently require this extended timeline and often stall by year three without delivering sustained improvements. BlueBin's turnkey approach eliminates this lengthy ramp-up period, delivering measurable transformation in 9 to 15 months through a comprehensive methodology that combines embedded coaching, proven processes, and strategic technology deployment. The question is whether you're willing to invest years hoping for improvement or achieve a documented 7.9x ROI in months.
The healthcare supply chain industry wastes $25.7 billion annually on preventable inefficiencies. Organizations implementing traditional in-house lean programs spend years building expertise, establishing processes, and training staff—only to discover that results remain elusive and commitment wanes. BJC HealthCare demonstrated an alternative path: a systematic transformation across 12 facilities, resulting in a 7 percent reduction in supply expenses, 30 percent efficiency gains, and $12.8 million in annual savings within 36 months. The difference lies not in the fundamentals of methodology but in execution discipline, implementation speed, and sustainability mechanisms.
The Year-3 Stall: Why Traditional Lean Programs Lose Momentum
AHRQ research on healthcare lean implementations reveals a consistent pattern: organizations begin with enthusiasm, achieve initial improvements, then experience significant momentum loss by the third year. This stall occurs so reliably that it represents a predictable failure mode rather than an exceptional circumstance.
The 3 to 5 Year Timeline Reality
Traditional lean program timelines reflect the learning curve organizations face when building expertise from scratch. Year one focuses on assessment, training, and pilot projects. Year two expands implementation while continuing to develop internal capabilities. Year three typically represents the point at which organizations either achieve sustainable transformation or experience a documented stall as enthusiasm wanes, champions move to new roles, and operational demands overwhelm improvement initiatives.
Healthcare systems pursuing internal lean transformation face multiple obstacles that extend timelines: building internal expertise requires extensive training and certification programs, implementing changes while maintaining operations creates competing priorities, ensuring consistent adoption across facilities demands substantial change management resources, and sustaining improvements requires ongoing coaching and accountability systems that organizations struggle to maintain.
The Hidden Cost of Extended Timelines
Every month spent preparing for transformation represents continued waste, excess inventory, clinical productivity losses, and missed financial opportunities. For an organization with $500 million annual supply spend, achieving a 7 percent reduction equals $35 million in annual savings. Delaying transformation by three years costs $105 million in foregone savings—far exceeding the investment required for turnkey implementation.
Beyond the direct financial impact, extended timelines lead to organizational fatigue. Initial enthusiasm gives way to skepticism as promised improvements remain distant. Clinical and supply chain staff become cynical about yet another improvement initiative. This cultural damage proves difficult to reverse, making future transformation efforts even more challenging.
BlueBin's Turnkey Approach: Eliminating the Ramp-Up Period
BlueBin's methodology delivers transformation 4x faster than traditional programs by providing complete expertise, proven processes, and embedded coaching from day one. Organizations don't build capability gradually over years—they deploy comprehensive solutions immediately through dedicated implementation teams.
The Five-Phase Transformation Process

BlueBin's proven transformation process follows a systematic methodology designed for speed without sacrificing sustainability:
Assess: Comprehensive evaluation of current supply chain operations, identifying waste sources, measuring baseline performance, engaging clinical stakeholders, and establishing transformation goals. This phase typically completes within weeks rather than months by deploying experienced assessment teams.
Design: Development of optimized supply configurations, PAR level establishment, workflow redesign, and system integration planning. Clinical engagement through mock events ensures designs support actual workflow patterns rather than theoretical ideals. Design phase leverages BlueBin's extensive experience across hundreds of implementations.
Embed: Implementation of 2-Bin Kanban methodology, BlueQ Analytics deployment, staff training, and BlueBelt certification. On-site transformation teams work directly with hospital staff five days per week, ensuring rapid knowledge transfer and adoption. Embedded coaching helps prevent the expertise gaps that can create delays in traditional programs.
Deploy: Systematic rollout across facilities, phased implementation that maintains operations, continuous optimization based on real-time data, and progressive scaling. BJC HealthCare's four-team deployment strategy demonstrates how large health systems achieve enterprise transformation within 36 months.
Sustain: Daily Management System implementation, Gemba audit processes, quarterly tune-ups, and ongoing BlueBelt development. These sustainability mechanisms prevent the year-3 stall by embedding a culture of continuous improvement and maintaining accountability structures beyond the initial implementation.
Dedicated Implementation Teams: The Speed Multiplier
BJC HealthCare's transformation demonstrates the power of dedicated teams. BlueBin deployed four implementation teams, each supported by BJC BlueBelt Program Specialists, conducting carefully orchestrated rollouts across 12 facilities. Each team cost $39,000 per month, a substantial investment that delivered exponential returns through accelerated implementation and guaranteed adoption.
These teams work on-site five days per week, providing immediate problem-solving, continuous training, real-time process optimization, and direct coaching. This intensive approach eliminates the stops and starts typical of internal programs where staff split time between transformation work and operational responsibilities.
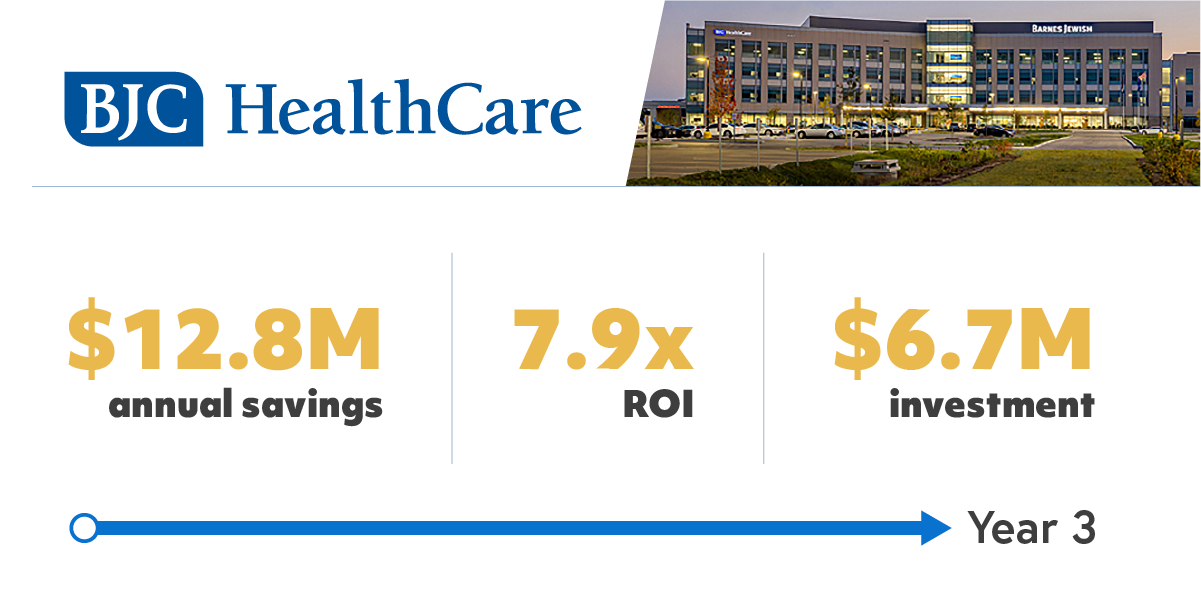
BJC HealthCare Case Study: Enterprise Transformation in 36 Months
BJC HealthCare, one of the largest nonprofit healthcare organizations in the United States, required a system-wide transformation of its supply chain. Their phased implementation demonstrates how large health systems achieve comprehensive change within timeframes that traditional approaches cannot match.
Phased Rollout Strategy
BJC's four-team deployment covered Missouri Baptist, Children's Hospital, St. Peter's, Barnes-Jewish Hospital Main, BJC West, Progress, Alton, Christian, Memorial, Memorial East, Parkland, and Sullivan. The systematic approach ensured each facility received dedicated attention while maintaining momentum across the enterprise.
Implementation progressed through 12-month phases, with teams conducting overlapping deployments that allowed knowledge sharing and best practice transfer. This phased strategy strikes a balance between speed and operational stability, preventing the chaos that often occurs when organizations attempt wholesale transformation without adequate support.
Investment Structure
BJC's comprehensive 36-month investment totaled $6.70 million:
- Implementation teams (four teams at $39,000 per month): $5.23 million
- Hardware (racks, bins, equipment): $1.36 million
- BlueQ Analytics ($7,000 per month): $252,000 over 36 months
This turnkey investment delivered a complete transformation, encompassing expertise, hardware, software, training, coaching, and guaranteed performance, thereby eliminating the hidden costs associated with trial and error typically found in internal programs.
Documented Financial Outcomes
BJC HealthCare achieved 7.9x ROI through:
- $12.8 million annual recurring savings at 3 percent supply expense reduction (potentially $21.4 million at 5 percent)
- $5.8 million one-time inventory reduction, releasing working capital
- $1.9 million annual resource redeployment value
- 7 percent supply expense reduction as a percentage of net patient revenue
- 30 percent supply chain operational efficiency gains
These outcomes emerged within 36 months, a significantly shorter timeframe than many organizations spend planning traditional lean initiatives. The documented ROI provided CFOs with concrete evidence of transformation value rather than promises of future improvement.

The Sustainability Difference: Preventing the Year-3 Stall
Achieving rapid transformation means nothing if improvements don't last. BlueBin's approach embeds sustainability mechanisms that prevent momentum loss, as seen in AHRQ documents, in traditional lean programs.
BlueBelt Certification: Building Internal Expertise
 BlueBelt certification offers a comprehensive 6- to 8-week training program that develops internal experts capable of sustaining and optimizing supply chain operations. Certified staff understand lean manufacturing principles, Kanban methodology, PAR optimization, Gemba audit processes, continuous improvement leadership, and data-driven decision making.
BlueBelt certification offers a comprehensive 6- to 8-week training program that develops internal experts capable of sustaining and optimizing supply chain operations. Certified staff understand lean manufacturing principles, Kanban methodology, PAR optimization, Gemba audit processes, continuous improvement leadership, and data-driven decision making.
BJC HealthCare's implementation included dedicated BlueBelt Program Specialists at each facility, ensuring expertise remained embedded in operations beyond initial deployment. This internal capacity prevents dependence on external consultants while maintaining the momentum of transformation.
Daily Management System: Systematic Accountability
The Daily Management System creates accountability structures that surface issues on the same day and drive continuous optimization. Daily huddles review performance metrics, address emerging problems, track improvement initiatives, and maintain focus on strategic goals. This systematic approach prevents the gradual drift that occurs when organizations lack structured management routines.
Weekly implementation huddles during rollout and quarterly steering sessions after deployment ensure alignment across organizational levels. This governance structure fosters executive engagement and eliminates barriers that could hinder progress.
Gemba Audits: Evidence-Based Improvement
Gemba audits, conducted where work actually happens, ensure adherence to standard work, identify process variations, recognize improvement opportunities, and engage staff in problem-solving. These systematic evaluations create feedback loops that drive ongoing refinement rather than allowing processes to deteriorate over time.
BlueQ Analytics provides data supporting Gemba findings, transforming subjective observations into quantifiable performance trends. This combination of direct observation and analytical validation enables evidence-based decision-making, a hallmark of mature continuous improvement programs.
The Financial Case for Speed: Calculating Delay Costs
Healthcare CFOs evaluating the timing of transformation should calculate the opportunity cost of delayed implementation. The financial impact becomes clear when analyzing foregone savings against investment requirements.
Comparative Timeline Analysis
Traditional Lean Program (5-Year Timeline):
- Year 1: Planning, training, pilot projects (minimal savings)
- Year 2: Expanded implementation (modest savings begin)
- Year 3: Momentum loss, potential stall (savings plateau)
- Year 4-5: Recovery attempts or program abandonment
- Total savings by Year 5: Uncertain, often minimal
BlueBin Turnkey Implementation (15-Month Timeline):
- Months 1-3: Assessment, design, initial deployment
- Months 4-9: Systematic rollout, immediate savings begin
- Months 10-15: Full implementation, documented outcomes
- Months 16-60: Sustained performance with embedded systems
- Total savings by Month 60: $64 million+ (BJC example)
ROI Timeline Comparison
Using BJC HealthCare's documented outcomes, organizations can project clear ROI timelines. At 15 months post-implementation, annual savings of $12.8 million begin accruing. By 36 months, cumulative savings reach $38.4 million against $6.70 million investment—delivering 5.7x return. By 60 months, cumulative savings exceed $64 million, representing 9.5x ROI.
Traditional programs that require 5 years to achieve comparable performance forfeit $51 million in savings during the extended ramp-up—capital that could fund other strategic initiatives, quality improvements, or financial reserves against market pressures.
Strategic Advantages Beyond Financial ROI
While financial outcomes justify investment, rapid transformation delivers strategic advantages that extend beyond ROI calculations.
Organizational Momentum and Cultural Change
Rapid results create organizational momentum that drives broader transformation. When clinical and supply chain staff experience immediate improvements, skepticism gives way to engagement. Success stories spread organically, building support for additional initiatives. This cultural shift—from cynicism about improvement programs to enthusiasm for evidence-based change—represents a value that no financial model can capture.
Competitive Positioning
Healthcare markets reward operational excellence. Organizations that achieve superior nurse satisfaction attract top talent. Systems that document strong financial performance secure favorable payer contracts. Facilities that demonstrate quality outcomes build a community's reputation. Supply chain transformation supporting these strategic objectives delivers competitive advantages that compound over time.
Risk Mitigation
Extended transformation timelines create implementation risk. Market conditions change, leadership transitions, priorities shift, and resources become constrained. Rapid deployment reduces exposure to these risks by delivering value before circumstances change, thereby mitigating the impact of unforeseen events. BlueBin's turnkey approach, with guaranteed performance, further mitigates risk by ensuring outcomes rather than relying on hope for success.
Implementation Considerations for Healthcare Systems
Healthcare executives evaluating transformation approaches should consider factors beyond implementation speed when comparing alternatives.
Scale and Complexity
BJC HealthCare's 12-facility implementation demonstrates scalability across large health systems. Smaller organizations achieve even faster results—single-facility implementations often complete within 9 to 12 months. The systematic methodology adapts to organizational size while maintaining quality and sustainability.
Operational Disruption Management
Concern about operational disruption during implementation represents a common barrier. BlueBin's phased approach explicitly addresses this concern through careful planning, parallel system operation during transition, dedicated on-site teams managing change, and immediate problem resolution that prevents workflow interruptions. Organizations maintain operations throughout transformation rather than experiencing the chaos some fear.
Executive Engagement Requirements
Successful transformation requires executive sponsorship but not excessive leadership time investment. BJC HealthCare's governance structure included quarterly steering sessions with executive sponsors, ensuring meaningful engagement without overwhelming executive schedules. This balanced approach ensures leadership alignment while allowing executives to focus on strategic priorities.
The Decision Framework: Speed Versus Extended Timelines
Healthcare organizations face a clear choice when addressing supply chain transformation: invest in turnkey implementation, delivering results in 9 to 15 months, or pursue traditional lean programs that require 3 to 5 years with uncertain outcomes. The financial analysis strongly favors rapid deployment. The strategic considerations reinforce this conclusion. The risk assessment eliminates remaining doubt.
Organizations cannot afford to waste time building capabilities that BlueBin provides immediately. Every month spent planning represents foregone savings, continued waste, and delayed competitive advantage. Rapid transformation is possible. BJC HealthCare and hundreds of other organizations prove it is. The question is whether executives will act decisively to capture available value or continue to accept inefficiency while hoping that traditional approaches will eventually deliver results.
FAQs
How does BlueBin achieve 4x faster implementation than traditional lean programs?
BlueBin eliminates the extended ramp-up period typically associated with traditional programs by providing comprehensive expertise, proven processes, and embedded coaching from day one. Dedicated implementation teams work on-site five days per week, conducting systematic Assessment, Design, Embed, Deploy, and Sustain phases. Organizations don't spend years building internal capabilities; they deploy comprehensive solutions immediately with guaranteed performance. BJC HealthCare achieved enterprise transformation across 12 facilities in 36 months, compared to the 3- to 5-year timeline outlined in AHRQ documents for traditional programs.
What causes the year-3 stall in traditional lean programs?
AHRQ research reveals a consistent momentum loss by year three in traditional lean programs, primarily due to waning enthusiasm, champions transitioning to new roles, operational demands overwhelming improvement initiatives, a lack of embedded expertise to sustain changes, and insufficient accountability structures. BlueBin prevents this stall through BlueBelt certification, building internal expertise, the Daily Management System, creating systematic accountability, Gemba audits, maintaining process adherence, and quarterly tune-ups, ensuring sustained optimization.
What is the financial cost of delaying supply chain transformation?
For an organization with $500 million annual supply spend, achieving a 7 percent reduction equals $35 million in annual savings. Delaying transformation by three years incurs $105 million in foregone savings, far exceeding the investment in turnkey implementation. BJC HealthCare's 36-month implementation resulted in $38.4 million in cumulative savings against a $6.70 million investment. Organizations pursuing 5-year traditional programs forfeit $51 million in savings during extended ramp-up while hoping for uncertain outcomes.
How does phased implementation work across large health systems?
BJC HealthCare's four-team deployment demonstrates enterprise scalability. BlueBin deploys dedicated teams conducting overlapping implementations across facilities in 12-month phases. Each team includes a Program Director, Program Manager, and Program Specialists, supported by facility BlueBelt champions. This systematic approach strikes a balance between implementation speed and operational stability, ensuring knowledge transfer between facilities, maintaining momentum across the enterprise, and adapting to facility-specific workflows while applying proven methodologies.
Can organizations achieve rapid transformation without operational disruption?
Yes. BlueBin's methodology specifically prevents operational disruption through careful, phased planning, parallel system operation during transition, dedicated on-site teams managing change on the same day, immediate problem resolution, and preventing workflow interruptions. Clinical engagement ensures designs support actual practice patterns. Organizations maintain operations throughout transformation. The Queen's Health System, BJC HealthCare, and hundreds of other implementations demonstrate that rapid deployment with proper support enables transformation without chaos.